Introduction
Hepatitis C is a viral infection that primarily impacts the liver, leading to inflammation and potential long-term health complications. With an estimated 71 million people worldwide living with chronic Hepatitis C, it remains a significant public health concern. This comprehensive guide aims to provide an in-depth understanding of Hepatitis C, including its causes, symptoms, diagnosis, treatment options, prevention strategies, and the importance of awareness and education surrounding this often-misunderstood disease.
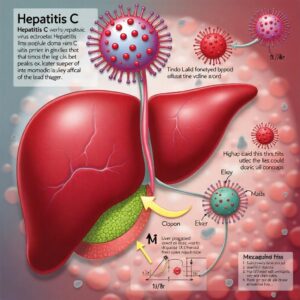
What is Hepatitis C?
Hepatitis C is caused by the Hepatitis C virus (HCV), which is transmitted through blood-to-blood contact. It can lead to chronic liver disease, cirrhosis, and liver cancer if left untreated. Understanding the virus and its implications is crucial for effective management and prevention.
Types of Hepatitis C
HCV is classified into several genotypes, which can influence treatment decisions. The most common genotypes include:
- Genotype 1: The most prevalent genotype in the United States and worldwide.
- Genotype 2: Less common, usually associated with a better response to treatment.
- Genotype 3: Often linked to more severe liver disease.
- Genotype 4: Predominantly found in the Middle East.
- Genotype 5: Rare, mostly seen in South Africa.
- Genotype 6: Common in Southeast Asia.
Understanding the specific genotype is crucial for tailoring treatment strategies effectively.
Causes of Hepatitis C
The primary cause of Hepatitis C is infection with the Hepatitis C virus. The virus is transmitted through:
Blood Transfusion
Receiving blood products before 1992, when screening for Hepatitis C began, significantly increases the risk of infection. Although rare today, the risk still exists in areas where blood screening is inadequate.
Intravenous Drug Use
One of the most significant risk factors for Hepatitis C is sharing needles or other drug paraphernalia. The Centers for Disease Control and Prevention (CDC) reports that approximately 60% of new infections occur among people who inject drugs.
Unprotected Sexual Contact
While less common, sexual transmission can occur, particularly in individuals with multiple partners or those who engage in high-risk sexual practices. The risk is higher among men who have sex with men and individuals with HIV.
From Mother to Child
Pregnant women with Hepatitis C can transmit the virus to their infants during childbirth. The risk of transmission is estimated to be around 5% to 6%.
Tattoos and Piercings
Using unsterilized equipment or receiving tattoos and piercings in unregulated environments can increase the risk of Hepatitis C transmission.
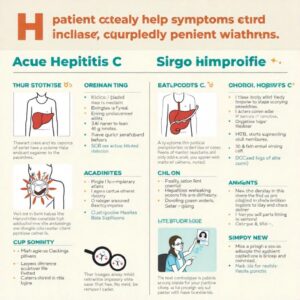
Symptoms of Hepatitis C
Many individuals with Hepatitis C may remain asymptomatic for years. However, when symptoms do occur, they can include:
Acute Phase Symptoms
In the early stages of infection, some individuals may experience mild symptoms, such as:
- Fatigue
- Nausea
- Loss of appetite
- Mild abdominal discomfort
- Jaundice (yellowing of the skin and eyes)
Chronic Phase Symptoms
If the infection becomes chronic, symptoms may become more pronounced and can include:
- Fatigue: Persistent tiredness that does not improve with rest.
- Jaundice: Yellowing of the skin and eyes due to liver dysfunction.
- Abdominal Pain: Discomfort or pain in the upper right abdomen.
- Loss of Appetite: Decreased desire to eat, which can lead to weight loss.
- Nausea and Vomiting: Digestive disturbances can occur.
- Dark Urine and Pale Stool: Changes in urine and stool color can indicate liver issues.
Complications of Hepatitis C
Chronic Hepatitis C can lead to severe health complications, including:
- Cirrhosis: Scarring of the liver that can occur over decades.
- Liver Cancer: Individuals with cirrhosis are at a much higher risk of developing liver cancer.
- Liver Failure: Advanced liver disease can lead to liver failure, requiring transplantation.
Diagnosis of Hepatitis C
Diagnosing Hepatitis C involves several steps:
Initial Screening
Blood tests are conducted to detect the presence of antibodies to HCV. If antibodies are detected, further testing is performed to confirm the diagnosis.
Confirmatory Testing
If antibodies are present, a follow-up test measures the viral load (the amount of virus in the blood). This test helps determine the severity of the infection.
Genotyping
Determining the strain of HCV can help guide treatment decisions. Different genotypes may respond differently to treatment.
Liver Assessment
Imaging tests (like ultrasound, CT scans, or MRI) or liver biopsy may be performed to assess liver damage and determine the extent of the disease. Non-invasive methods, such as elastography, can also be used to evaluate liver stiffness.
Treatment Options for Hepatitis C
The treatment landscape for Hepatitis C has evolved significantly in recent years. The following options are commonly used:
Direct-Acting Antivirals (DAAs)
DAAs are the most effective treatment for Hepatitis C. They work by targeting specific steps in the HCV life cycle, leading to a sustained virologic response (SVR), which means the virus is undetectable in the blood after treatment. Common DAAs include:
- Sofosbuvir: Often used in combination with other medications.
- Ledipasvir: Typically combined with Sofosbuvir.
- Velpatasvir: Used for various genotypes of HCV.
- Glecaprevir/Pibrentasvir: A pan-genotypic treatment option.
Treatment Duration
The duration of treatment varies based on the genotype of the virus, the presence of liver damage, and previous treatment history. Most courses last between 8 to 12 weeks, though some patients may require longer treatment.
Side Effects
While DAAs are generally well-tolerated, some individuals may experience side effects, including:
- Fatigue
- Headache
- Nausea
- Insomnia
Importance of Adherence
Adhering to the prescribed treatment regimen is crucial for achieving a cure. Missing doses can lead to treatment failure and the development of drug-resistant strains.
Living with Hepatitis C
For those diagnosed with Hepatitis C, lifestyle changes can help manage the condition:
Healthy Diet
Eating a balanced diet can support liver health. A diet rich in fruits, vegetables, whole grains, and lean proteins is recommended. Avoiding high-fat, high-sugar, and processed foods can also be beneficial.
Regular Exercise
Physical activity can improve overall well-being and help maintain a healthy weight, which is essential for liver health.
Avoid Alcohol
Alcohol can exacerbate liver damage and should be avoided. Individuals with Hepatitis C should consult with their healthcare provider about safe consumption levels.
Regular Medical Check-ups
Ongoing monitoring and treatment are essential. Regular appointments with a healthcare provider can help manage the disease and monitor liver health.
Mental Health Support
Living with a chronic illness can be challenging. Seeking support from mental health professionals, support groups, or counseling can help individuals cope with the emotional aspects of living with Hepatitis C.
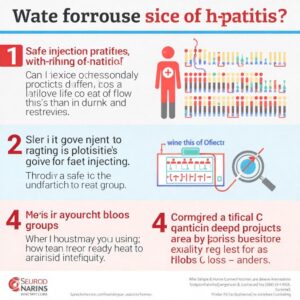
Prevention of Hepatitis C
Preventing Hepatitis C involves several strategies:
Avoid Sharing Needles
Individuals who use intravenous drugs should not share needles or equipment. Needle exchange programs can provide safe alternatives.
Safe Sexual Practices
Using condoms can reduce the risk of transmission during sexual activity. Open discussions about sexual health with partners can also help mitigate risks.
Screening Blood Products
Ensuring blood products are screened for HCV before transfusion is crucial. Most countries have stringent regulations to prevent transmission through blood products.
Safe Tattooing and Piercing
Ensure that all equipment is sterile and that reputable establishments are used for tattoos and piercings. Always ask about sterilization practices.
Education and Awareness
Raising awareness about Hepatitis C and its transmission routes can help reduce stigma and encourage individuals to seek testing and treatment.
The Importance of Awareness and Education
Raising awareness about Hepatitis C is crucial for prevention and early detection. Many individuals are unaware of their infection status, leading to delayed diagnosis and treatment. Public health campaigns can help educate individuals about the risks, symptoms, and importance of regular testing.
Community Engagement
Community organizations play a vital role in promoting awareness and providing resources for individuals at risk. Educational workshops, outreach programs, and health fairs can help disseminate information about Hepatitis C.
The Role of Healthcare Providers
Healthcare providers should routinely screen individuals at risk for Hepatitis C, especially those with a history of intravenous drug use, unprotected sex, or prior blood transfusions. Educating patients about the disease and available treatment options can empower them to take control of their health.
FAQs about Hepatitis C
1. Can Hepatitis C be cured?
Yes, Hepatitis C can be cured with appropriate antiviral treatment. Most individuals achieve a sustained virologic response after completing treatment.
2. How is Hepatitis C diagnosed?
Diagnosis involves blood tests to detect antibodies to HCV and confirmatory tests to measure the viral load.
3. What are the symptoms of Hepatitis C?
Symptoms can include fatigue, jaundice, abdominal pain, loss of appetite, nausea, and changes in urine and stool color.
4. How can I prevent Hepatitis C?
Preventative measures include avoiding sharing needles, practicing safe sex, ensuring blood products are screened, and using sterile equipment for tattoos and piercings.
5. What treatments are available for Hepatitis C?
Direct-acting antivirals (DAAs) are the primary treatment option and have a high cure rate.
6. Are there any long-term effects of Hepatitis C?
Chronic Hepatitis C can lead to severe health complications, including cirrhosis, liver cancer, and liver failure.
7. Is Hepatitis C contagious?
Yes, Hepatitis C is contagious and is primarily transmitted through blood-to-blood contact.
8. Can I live a normal life with Hepatitis C?
Yes, with proper treatment and lifestyle management, individuals with Hepatitis C can lead healthy and fulfilling lives.
Conclusion
Hepatitis C remains a critical public health issue, but advancements in treatment and prevention offer hope for those affected. Understanding the virus, its transmission, and effective management strategies can empower individuals to take control of their health. If you suspect you may have been exposed to Hepatitis C, seek medical advice promptly for testing and potential treatment. Raising awareness and educating others about Hepatitis C is essential in combating this disease and supporting those living with it.
Data Sources to Reference
- World Health Organization (WHO) – Hepatitis C Factsheet
- Centers for Disease Control and Prevention (CDC) – Hepatitis C Information
- American Association for the Study of Liver Diseases (AASLD) – Guidelines for Treatment of Hepatitis C
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – Hepatitis C Overview
- Hepatitis C Support Project – Resources for Patients and Caregivers

1 thought on “Hepatitis C: A Comprehensive Guide”