Introduction:
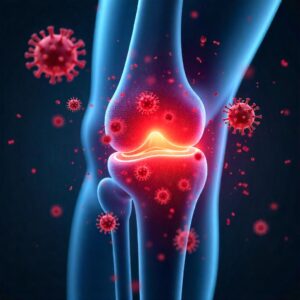
Rheumatoid arthritis (RA) is a chronic autoimmune disease that primarily affects the joints. It causes inflammation, pain, swelling, and eventually joint damage if left untreated. Unlike osteoarthritis, which results from wear and tear, RA occurs when the immune system mistakenly attacks the body’s own tissues.
RA affects over 1.3 million Americans and millions more worldwide. It can significantly impact a person’s quality of life, leading to disability and other complications if not properly managed. This comprehensive guide explores the causes, symptoms, diagnosis, and treatment options for rheumatoid arthritis, helping patients and caregivers understand and manage the disease effectively.
What is Rheumatoid Arthritis?
Rheumatoid arthritis is a systemic autoimmune disorder. It mainly targets the synovium, the lining of the membranes that surround your joints. The immune system, instead of protecting the body, attacks this lining, resulting in inflammation and thickening of the synovium. Over time, this can destroy cartilage and bone within the joint.
RA is symmetrical, meaning it typically affects joints on both sides of the body, such as both wrists, knees, or hands. It can also affect other organs, including the eyes, lungs, and heart.
Causes of Rheumatoid Arthritis
The exact cause of rheumatoid arthritis is unknown, but several factors are believed to contribute to its development:
1. Genetics
Family history plays a significant role. People with certain genes, such as HLA-DR4, are more likely to develop RA.
2. Autoimmune Response
RA is an autoimmune condition, meaning the immune system mistakenly attacks healthy tissue, particularly the joints.
3. Environmental Factors
Exposure to certain environmental triggers, such as smoking, asbestos, or silica, can increase the risk of developing RA.
4. Sex and Hormones
Women are three times more likely to develop RA than men. Hormonal changes during pregnancy or menopause may influence disease onset or progression.

5. Infections
Some studies suggest that infections may trigger RA in genetically susceptible individuals, although no specific pathogen has been confirmed.
Symptoms of Rheumatoid Arthritis
RA symptoms often develop gradually and worsen over time. They can vary in severity and may come and go in flares.
Common Symptoms Include:
- Joint pain and swelling
- Morning stiffness, lasting more than 30 minutes
- Fatigue
- Fever
- Weight loss
- Warm, tender joints
- Decreased range of motion
Early Symptoms:
- Subtle joint discomfort, especially in fingers and toes
- Fatigue or malaise
- Mild fever
Advanced Symptoms:
- Joint deformity
- Loss of joint function
- Rheumatoid nodules
- Eye and lung involvement
Stages of Rheumatoid Arthritis
RA progresses through the following stages:
- Stage 1 (Early RA): Inflammation causes joint pain and swelling.
- Stage 2 (Moderate RA): Inflammation damages cartilage.
- Stage 3 (Severe RA): Damage extends to bone, causing deformities.
- Stage 4 (End-stage RA): Joints stop functioning; pain may lessen, but mobility is severely limited.
How is Rheumatoid Arthritis Diagnosed?
Diagnosing RA involves a combination of physical exams, lab tests, and imaging studies.
1. Physical Examination
Doctors check for swelling, redness, and warmth in the joints, along with range of motion and tenderness.
2. Blood Tests
- Rheumatoid Factor (RF): An antibody found in ~70% of RA patients.
- Anti-CCP Antibodies: More specific for RA.
- Erythrocyte Sedimentation Rate (ESR) and C-reactive protein (CRP): Indicate inflammation.
3. Imaging Tests
- X-rays: Detect joint damage over time.
- Ultrasound and MRI: Show early joint inflammation and erosion.

Treatment Options for Rheumatoid Arthritis
Early and aggressive treatment is key to managing RA. The goal is to reduce inflammation, relieve symptoms, prevent joint damage, and improve quality of life.
1. Medications
a. Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
Reduce pain and inflammation but do not slow disease progression.
b. Corticosteroids
Quick relief of inflammation; used short-term due to side effects.
c. Disease-Modifying Antirheumatic Drugs (DMARDs)
Slow disease progression by modifying the immune response.
- Examples: Methotrexate, Sulfasalazine, Leflunomide
d. Biologic Agents
Target specific parts of the immune system. Used when DMARDs are ineffective.
- Examples: Etanercept, Adalimumab, Rituximab
e. Janus Kinase (JAK) Inhibitors
Oral medications that block inflammatory signaling pathways.
- Examples: Tofacitinib, Baricitinib
2. Physical and Occupational Therapy
Therapists help maintain joint function, improve mobility, and recommend assistive devices.
3. Surgery
In severe RA, joint replacement or reconstruction may be necessary.
- Synovectomy: Removal of inflamed synovium
- Tendon repair
- Joint fusion or replacement
Lifestyle and Home Remedies
1. Exercise
Low-impact activities like swimming, walking, and yoga improve strength and flexibility.
2. Healthy Diet
A rheumatoid arthritis diet rich in omega-3 fatty acids, antioxidants, and fiber can reduce inflammation.
Foods to Eat:
- Fatty fish (salmon, mackerel)
- Leafy greens
- Whole grains
- Berries
- Nuts and seeds
Foods to Avoid:
- Processed foods
- Sugary drinks
- Red meat
- Refined carbohydrates
3. Stress Management
Stress can worsen RA symptoms. Techniques like meditation, deep breathing, and counseling can help.
4. Quit Smoking
Smoking is a major risk factor for RA and worsens disease outcomes.
Complications of Rheumatoid Arthritis
If untreated or poorly managed, RA can lead to:
- Joint deformity and disability
- Osteoporosis
- Rheumatoid nodules
- Heart disease
- Lung disease
- Infections
- Lymphoma
Living with Rheumatoid Arthritis
Living with RA requires a proactive and comprehensive approach. Here are some tips:
1. Follow Your Treatment Plan
Adherence to medications and appointments is essential for disease control.
2. Monitor Symptoms
Keep a journal of symptoms, medication side effects, and flare triggers.
3. Use Joint Protection Techniques
Avoid repetitive motions, use assistive devices, and modify daily tasks to protect joints.
4. Stay Informed
Educate yourself about RA and connect with support groups or online communities.
Rheumatoid Arthritis and Mental Health
Chronic illness like RA can lead to depression, anxiety, and social isolation. Mental health support is vital.
- Talk to a therapist or counselor
- Join RA support groups
- Practice mindfulness and self-care
Alternative and Complementary Therapies
While not a replacement for medical treatment, some patients find relief through:
- Acupuncture
- Massage therapy
- Tai chi
- Supplements (e.g., turmeric, fish oil)
Always consult your doctor before starting any alternative therapy.
Current Research and Future Outlook
Exciting advances in RA research include:
- Personalized medicine based on genetic profiles
- New biologics targeting novel immune pathways
- Early diagnostic tools to detect RA before symptoms appear
With ongoing research, the future of RA treatment is promising, focusing on remission and long-term management.
Conclusion
Rheumatoid arthritis is a serious, chronic autoimmune disease that requires early detection and a multifaceted treatment approach. Through a combination of medications, lifestyle changes, therapy, and support, individuals with RA can live active, fulfilling lives.
If you suspect you have RA, consult a rheumatologist as early treatment can significantly improve outcomes. Stay informed, stay active, and take control of your health.
Frequently Asked Questions (FAQs)
1. Is rheumatoid arthritis curable?
RA is not curable, but it is manageable with proper treatment and lifestyle changes.
2. What are the early warning signs of RA?
Common early signs include joint stiffness (especially in the morning), fatigue, and mild joint swelling.
3. Can diet affect rheumatoid arthritis?
Yes, a healthy anti-inflammatory diet can help manage RA symptoms and improve overall well-being.
4. Who is at risk for developing RA?
Women, smokers, and those with a family history of RA are at higher risk.
5. What is the life expectancy of someone with RA?
With proper treatment, many people with RA live a normal life span. However, severe, uncontrolled RA can reduce life expectancy.
Meta Description: Learn everything about rheumatoid arthritis (RA) including its causes, symptoms, diagnosis, treatment options, diet tips, and how to manage it effectively for a better quality of life.


1 thought on “Rheumatoid Arthritis: Causes, Symptoms, Diagnosis, and Treatment”