Introduction
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that primarily affects the colon and rectum. Characterized by inflammation and ulceration of the intestinal lining, ulcerative colitis can significantly impact the quality of life for those affected. This blog post aims to provide an in-depth understanding of ulcerative colitis, covering its causes, symptoms, diagnosis, treatment options, lifestyle management strategies, and the latest research in the field.

Keywords: Ulcerative Colitis, Inflammatory Bowel Disease, Symptoms, Diagnosis, Treatment, Lifestyle Management, Risk Factors, Complications, Nutrition
What is Ulcerative Colitis?
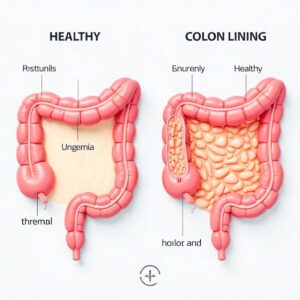
Ulcerative colitis is a type of inflammatory bowel disease (IBD) that causes long-lasting inflammation and ulcers in the digestive tract. It primarily affects the innermost lining of the colon and rectum, leading to various gastrointestinal symptoms.
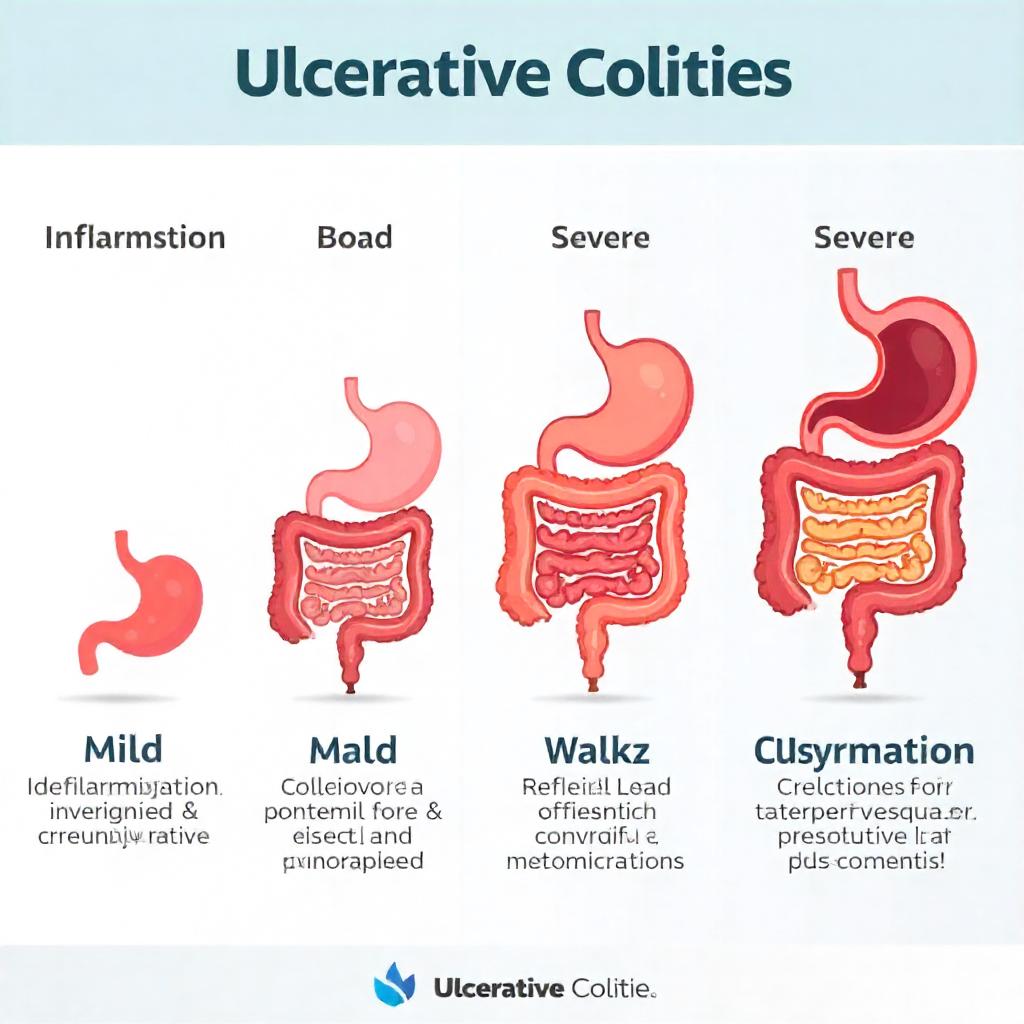
Types of Ulcerative Colitis
- Ulcerative Proctitis: This form affects only the rectum and is often mild. Symptoms usually include rectal bleeding and discomfort.
- Proctosigmoiditis: Involves the rectum and the lower part of the colon (sigmoid colon). Symptoms may include diarrhea, abdominal pain, and rectal bleeding.
- Left-sided Colitis: Extends from the rectum to the upper part of the colon (splenic flexure). Symptoms include abdominal pain on the left side, diarrhea, and weight loss.
- Pancolitis: Affects the entire colon. Symptoms are more severe and can include significant weight loss, severe diarrhea, and fatigue.
- Acute Severe Ulcerative Colitis: A rare but serious form that can lead to life-threatening complications. Symptoms include severe abdominal pain, persistent vomiting, and dehydration.
Causes of Ulcerative Colitis
The exact cause of ulcerative colitis is not fully understood. However, several factors may contribute to its development:
1. Genetics
Family history may play a role, as ulcerative colitis tends to run in families. Studies have shown that individuals with a first-degree relative diagnosed with UC are at a higher risk of developing the condition.
2. Immune System
An abnormal immune response may lead to chronic inflammation in the digestive tract. In people with ulcerative colitis, the immune system mistakenly attacks healthy cells in the colon, resulting in inflammation and ulceration.
3. Environmental Factors
Certain environmental factors, such as diet, stress, and exposure to certain medications or infections, may trigger or worsen symptoms. Some studies suggest that a diet high in processed foods and low in fiber may contribute to the development of ulcerative colitis.
4. Microbiome Imbalance
The gut microbiome, which consists of trillions of bacteria and other microorganisms, plays a crucial role in digestion and immune function. An imbalance in the gut microbiome may contribute to the development of ulcerative colitis.
Symptoms of Ulcerative Colitis
Symptoms of ulcerative colitis can vary in severity and may come and go over time. Common symptoms include:
- Abdominal Pain and Cramping: Pain is often located in the lower abdomen and may be accompanied by cramping.
- Diarrhea: Frequent bowel movements may occur, often with blood or pus. The urgency to defecate can be overwhelming, leading to discomfort.
- Urgency to Defecate: Individuals may feel a sudden, strong need to have a bowel movement, which can be distressing.
- Fatigue: Chronic inflammation may lead to fatigue and a general feeling of malaise.
- Weight Loss: Unintentional weight loss may occur due to decreased appetite and nutrient malabsorption.
- Loss of Appetite: Many individuals experience a reduced desire to eat, which can contribute to weight loss.
- Fever: Low-grade fever may accompany flare-ups, indicating inflammation in the body.
Complications
While ulcerative colitis can be managed, it may lead to complications such as:
- Severe Dehydration: Frequent diarrhea can lead to significant fluid loss and dehydration.
- Toxic Megacolon: This rare but life-threatening condition involves extreme dilation of the colon and can lead to perforation.
- Colon Cancer: Long-term inflammation increases the risk of developing colorectal cancer, especially in individuals with pancolitis.
- Joint Pain: Some people with ulcerative colitis may experience joint pain or arthritis.
- Skin Disorders: Skin rashes or lesions may occur as a result of the inflammatory process.
- Liver Disease: Conditions such as primary sclerosing cholangitis (PSC) may develop, leading to liver damage.

Diagnosis of Ulcerative Colitis
Diagnosing ulcerative colitis involves a combination of medical history, physical examination, and diagnostic tests.
1. Medical History and Symptoms
A healthcare provider will inquire about symptoms, family history of inflammatory bowel diseases, and any previous gastrointestinal issues.
2. Physical Examination
A physical exam may help identify signs of inflammation, tenderness in the abdomen, or complications such as bloating.
3. Diagnostic Tests
- Colonoscopy: The primary diagnostic tool, allowing direct visualization of the colon and rectum. During the procedure, the doctor can take biopsies to confirm the diagnosis.
- Biopsy: Tissue samples may be taken during colonoscopy to confirm ulcerative colitis and rule out other conditions.
- Imaging Tests: CT scans or MRIs may be used to assess the extent of inflammation and rule out complications.
- Blood Tests: Blood tests can help identify anemia, inflammation markers, and electrolyte imbalances.
- Stool Tests: These tests can help rule out infections and assess for inflammation in the intestines.
Treatment Options for Ulcerative Colitis
Treatment for ulcerative colitis aims to reduce inflammation, manage symptoms, and achieve remission.
1. Medications
a. Aminosalicylates
These medications, such as mesalamine, are often the first line of treatment for mild to moderate ulcerative colitis. They work by reducing inflammation in the lining of the intestines.
b. Corticosteroids
Corticosteroids, such as prednisone, may be prescribed for short-term relief of severe inflammation. However, they are not recommended for long-term use due to potential side effects.
c. Immunosuppressants
Medications like azathioprine and mercaptopurine suppress the immune response to reduce inflammation. These may be used in combination with other treatments.
d. Biologics
Targeted therapies, such as infliximab and adalimumab, block specific pathways in the inflammatory process. Biologics are often recommended for moderate to severe ulcerative colitis or for individuals who do not respond to other treatments.
e. Janus Kinase Inhibitors
Tofacitinib is a newer class of medication that inhibits specific pathways involved in inflammation.
2. Lifestyle Modifications
a. Diet
- Identify Trigger Foods: Keeping a food diary can help identify foods that worsen symptoms. Common triggers include dairy, high-fat foods, spicy foods, and caffeine.
- Stay Hydrated: Drink plenty of fluids, especially during flare-ups, to prevent dehydration.
- Balanced Diet: Focus on a nutrient-rich diet that includes fruits, vegetables, lean proteins, and whole grains (if tolerated).
b. Stress Management
Stress can exacerbate symptoms of ulcerative colitis. Techniques such as meditation, yoga, deep breathing exercises, and regular physical activity can help manage stress levels.
c. Regular Exercise
Engaging in regular physical activity can improve overall health and well-being. Exercise may help reduce stress and promote better digestive health.
3. Surgery
In severe cases of ulcerative colitis that do not respond to medical treatment, surgical options may be considered. Surgical options include:
- Colectomy: This procedure involves the removal of the colon. In some cases, a pouch (ileal pouch-anal anastomosis) is created from the small intestine to allow for normal bowel function without a permanent colostomy.
- Ileostomy: If a colectomy is performed, an ileostomy may be necessary, creating an opening in the abdominal wall to allow waste to exit the body into a pouch.

Lifestyle Management for Ulcerative Colitis
Living with ulcerative colitis requires ongoing management and lifestyle adjustments. Here are some strategies to consider:
1. Dietary Changes
- Identify Trigger Foods: Keep a food diary to track symptoms and identify problematic foods. Work with a dietitian to create a personalized meal plan.
- Stay Hydrated: Drink plenty of fluids, especially during flare-ups. Electrolyte drinks may be beneficial to replenish lost nutrients.
- Low Residue Diet: During flare-ups, a low-residue diet may help minimize symptoms by reducing the amount of undigested food that passes through the intestines.
2. Regular Check-ups
Schedule regular appointments with a gastroenterologist to monitor the condition and adjust treatment as necessary. Regular colonoscopies may be recommended to screen for colon cancer, especially for those with long-standing ulcerative colitis.
3. Support Groups
Join support groups or online communities to connect with others facing similar challenges. Sharing experiences and coping strategies can provide emotional support and reduce feelings of isolation.
4. Mental Health Support
Living with a chronic condition can take a toll on mental health. Consider seeking support from a therapist or counselor who specializes in chronic illness. Cognitive-behavioral therapy (CBT) may be particularly effective in managing anxiety and depression related to ulcerative colitis.
5. Education
Educate yourself about ulcerative colitis and stay informed about the latest research and treatment options. Understanding your condition can empower you to make informed decisions about your health and treatment.
The Latest Research and Advances in Ulcerative Colitis
Research on ulcerative colitis is ongoing, with new treatment options and insights being developed regularly. Some of the latest advancements include:
1. Personalized Medicine
Researchers are exploring personalized treatment approaches based on genetic and molecular profiling. This may lead to more targeted therapies that are tailored to individual patients.
2. Microbiome Research
Studies are investigating the role of the gut microbiome in ulcerative colitis. Probiotics and dietary interventions aimed at restoring gut microbiota may hold promise in managing the condition.
3. New Medications
Several new medications are under investigation, including small molecules and biologics that target specific pathways involved in inflammation. These may offer new options for patients who do not respond to existing treatments.
4. Surgical Techniques
Advancements in surgical techniques, including minimally invasive approaches, are improving outcomes for patients requiring surgery for ulcerative colitis.
FAQs about Ulcerative Colitis
Q1: Is ulcerative colitis curable?
A1: Currently, there is no cure for ulcerative colitis, but it can be managed effectively with medication and lifestyle changes. Some individuals may experience long periods of remission.
Q2: Can diet affect ulcerative colitis?
A2: Yes, certain foods may trigger symptoms. It’s important to identify and avoid these triggers while maintaining a balanced diet that supports overall health.
Q3: What are the long-term effects of ulcerative colitis?
A3: Long-term effects can include an increased risk of colon cancer, complications such as toxic megacolon, and potential impacts on mental health.
Q4: How is ulcerative colitis different from Crohn’s disease?
A4: While both are types of inflammatory bowel disease, ulcerative colitis primarily affects the colon, whereas Crohn’s disease can affect any part of the gastrointestinal tract.
Q5: What lifestyle changes can help manage ulcerative colitis?
A5: Dietary modifications, stress management techniques, regular exercise, and staying hydrated can help manage symptoms and improve quality of life.
Q6: Are there any alternative therapies for ulcerative colitis?
A6: Some individuals explore alternative therapies such as acupuncture, herbal supplements, or yoga. However, it’s essential to consult with a healthcare provider before starting any alternative treatments.
Conclusion
Ulcerative colitis is a chronic condition that requires comprehensive management and understanding. By recognizing the symptoms, seeking timely diagnosis, and adhering to treatment plans, individuals with ulcerative colitis can lead fulfilling lives. Ongoing research continues to enhance our understanding of this condition, promising better management strategies and potential future therapies.
References
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Available at: NIDDK
- Mayo Clinic. Available at: Mayo Clinic
- Crohn’s & Colitis Foundation. Available at: Crohn’s & Colitis Foundation
- American Gastroenterological Association. Available at: AGA
- Research articles from journals such as Gastroenterology and Inflammatory Bowel Diseases.

1 thought on “Ulcerative Colitis: A Comprehensive Guide”